Stem Cell Therapy - the improved diagnostics available to treat lameness
Article by Jackie Zions (interviewing Dr. Koenig)
Prevention is the ideal when it comes to lameness, but practically everyone who has owned horses has dealt with a lay-up due to an unforeseen injury at some point. The following article will provide tools to sharpen your eye for detecting lameness, review prevention tips and discuss the importance of early intervention. It will also begin with a glimpse into current research endeavouring to heal tendon injuries faster, which has obvious horse welfare benefits and supports horse owners eager to return to their training programs. Dr. Judith Koenig of Ontario Veterinary College (OVC) spends half of her time as a surgeon and teacher with a strong interest in equine sports medicine and rehabilitation, and the other half as a researcher at the OVC.
Lameness is a huge focus for Koenig, whose main interest is in tissue healing. “I think over the past 20 or 30 years we have become very, very good at diagnosing the cause of lameness,” says Koenig. “In the past, we had only radiographs and ultrasound as a diagnostic tool, but by now most referral centres also have MRI available; and that allows us to diagnose joint disease or tendon disease even more. We are much better now [at] finding causes that previously may have been missed with ultrasound.”
Improvements in diagnostics have resulted in increased ability to target treatment plans. With all the different biologics on the market today, Koenig sees a shift in the management of joint disease with more people getting away from steroids as a treatment.
The following list is excerpted from Equine Guelph’s short course on lameness offered on TheHorsePortal.ca. It outlines the different diagnostics available:
When asked for the latest news on research she has been involved in, Koenig proclaims, “I'm most excited about the fact that horses are responding well to stem cell treatment—better than I have seen any response to any other drug we have tried so far!”
Koenig has investigated the use of many different modalities to see if they accelerate tissue healing and has studied which cellular pathways are affected. Two recent collaborative studies have produced very exciting findings, revealing future promise for treating equine osteoarthritis with stem cell therapy.
In a safety study, Koenig and her team at the Ontario Veterinary College have shown equine pooled cryopreserved umbilical cord blood, (eCB) MSC, to be safe and effective in treatment of osteoarthritis.
“These cells are the ones harvested from umbilical cord blood at the time of foaling and then that blood is taken to the lab and the stem cells are isolated out of it,” explains Koenig. The stem cells are then put through a variety of tests to make sure they are free of infectious diseases. Once given a clean bill of health, they are expanded and frozen.
The stem cells harvested from multiple donors of equine umbilical cord blood [eCB, (kindly provided by eQcell), MSC] were compared to saline injections in research horses. “This type of cells is much more practical if you have a cell bank,” says Koenig. “You can treat more horses with it, and it’s off the shelf.” There were no systemic reactions in the safety study. Research has also shown no different reactions from sourcing from one donor or multiple donors.
In the second study, 10 million stem cells per vial were frozen for use in healing OA from fetlock chips in horses that were previously conditioned to be fit. After the fetlock chip was created, exercise commenced for six more weeks, and then osteoarthritis was evaluated by MRI for a baseline. Half the horses were treated with the pooled MSC stem cells, and the control group received saline before another month of exercise. Then MRI and lameness exams were repeated, and arthroscopy was repeated to score the cartilage and remove the chip.
Lameness was decreased and cartilage scores were improved in the group that received stem cell therapy at the time of the second look with arthroscopy.
Many diagnostics were utilised during this study. MRIs, X-rays, ultrasounds and weekly lameness evaluations all revealed signs of osteoarthritis in fetlock joints improved in the group treated with (eCB) MSCs. After six weeks of treatment, the arthroscopic score was significantly lower (better cartilage) in the MSC group compared to the control group.
“Using the MRI, we can also see a difference that the horses treated with stem cells had less progression of osteoarthritis, which I think is awesome,” says Koenig. “They were less lame when exercised after the stem cell therapy than the horses that received saline.”
This research group also just completed a clinical trial in client-owned horses diagnosed with fetlock injuries with mild to moderate osteoarthritis changes. The horses were given either 10 million or 20 million stem cells and rechecked three weeks and six weeks after the treatment. Upon re-evaluation, the grade of lameness improved in all the horses by at least one. Only two horses presented a mild transient reaction, which dissipated after 48 hours without any need for antibiotics. The horse’s joints looked normal, with any filling in the joint reduced.
There was no difference in the 18 horses, with nine given 10 million stem cells and the other nine 20 million stem cells; so in the next clinical trial, 10 million stem cells will be used.
The research team is very happy with the results of this first-of-its-kind trial, proving that umbilical cord blood stem cells stopped the progression of osteoarthritis and that the cartilage looked better in the horses that received treatment. The future of stem cell therapy is quite promising!
Rehabilitation
Research has shown adhering to a veterinary-prescribed rehabilitation protocol results in a far better outcome than paddock turn out alone. It is beneficial for tendon healing to have a certain amount of controlled stimulation. “These horses have a much better outcome than the horses that are treated with just being turned out in a paddock for half a year,” emphasises Koenig. “They do much better if they follow an exercise program. Of course, it is important not to overdo it.”
For example, Koenig cautions against skipping hand-walking if it has been advised. It can be so integral to stimulating healing, as proven in recent clinical trials. “The people that followed the rehab instructions together with the stem cell treatment in our last study—those horses all returned to racing,” said Koenig.
“It is super important to follow the rehab instructions when it comes to how long to rest and not to start back too early.”
Another concern when rehabilitating an injured horse would be administering any home remedies that you haven't discussed with your veterinarian. Examples included blistering an area that is actively healing or applying shockwave to mask pain and then commence exercise.
Prevention and Training Tips
While stating there are many methods and opinions when it comes to training horses, Koenig offered a few common subjects backed by research. The first being the importance of daily turnout for young developing horses.
Turnout and exercise
Many studies have looked at the quality of cartilage in young horses with ample access to turn out versus those without. It has been determined that young horses that lack exercise and are kept in a stall have very poor quality cartilage.
Horses that are started early with light exercise (like trotting short distances and a bit of hill work) and that have access to daily paddock turnout, had much better quality of cartilage. Koenig cited research from Dr. Pieter Brama and similar research groups.
Another study shows that muscle and tendon development depend greatly on low grade exercise in young horses. Evaluations at 18 months of age found that the group that had paddock turnout and a little bit of exercise such as running up and down hills had better quality cartilage, tendon and muscle.
Koenig provides a human comparison, with the example of people that recover quicker from injury when they have been active as teenagers and undergone some beneficial conditioning. The inference can be made that horses developing cardiovascular fitness at a young age stand to benefit their whole lives from the early muscle development.
Koenig says it takes six weeks to regain muscle strength after injury, but anywhere from four to six months for bone to develop strength. It needs to be repeatedly loaded, but one should not do anything too crazy! Gradual introduction of exercise is the rule of thumb.
Rest and Recovery
“Ideally they have two rest days a week, but one rest day a week as a minimum,” says Koenig. “I cannot stress enough the importance of periods of rest after strenuous work, and if you notice any type of filling in the joints after workout, you should definitely rest the horse for a couple of days and apply ice to any structures that are filled or tendons or muscles that are hard.”
Not purporting to be a trainer, Koenig does state that two speed workouts a week would be a maximum to allow for proper recovery. You will also want to make sure they have enough access to salt/electrolytes and water after training.
During a post-Covid interview, Koenig imparted important advice for bringing horses back into work methodically when they have experienced significant time off.
“You need to allow at least a six-week training period for the athletes to be slowly brought back and build up muscle mass and cardiovascular fitness,” says Koenig. “Both stamina and muscle mass need to be retrained.”
Watch video: “Lameness research - What precautions do you take to start training after time off?” https://www.youtube.com/watch?v=zNHba_nXi2k
The importance was stressed to check the horse’s legs for heat and swelling before and after every ride and to always pick out the feet. A good period of walking is required in the warmup and cool down; and riders need to pay attention to soundness in the walk before commencing their work out.
Footing and Cross Training
With a European background, Koenig is no stranger to the varying track surfaces used in their training programs. Statistics suggest fewer injuries with horses that are running on turf.
Working on hard track surfaces has been known to increase the chance of injury, but delving into footing is beyond the scope of this article.
“Cross training is very important,” says Koenig. “It is critical for the mental and proper musculoskeletal development of the athlete to have for every three training days a day off, or even better provide cross-training like trail riding on these days."
Cross-training can mitigate overtraining, giving the body and mind a mental break from intense training. It can increase motivation and also musculoskeletal strength. Varied loading from training on different terrain at different gaits means bone and muscle will be loaded differently, therefore reducing repetitive strain that can cause lameness.
Hoof care
Whether it is a horse coming back from injury, or a young horse beginning training, a proficient farrier is indispensable to ensure proper balance when trimming the feet. In fact, balancing the hoof right from the start is paramount because if they have some conformational abnormalities, like abnormal angles, they tend to load one side of their joint or bone more than the other. This predisposes them to potentially losing bone elasticity on the side they load more because the bone will lay down more calcium on that side, trying to make it stronger; but it actually makes the bone plate under the cartilage brittle.
Koenig could not overstate the importance of excellent hoof care when it comes to joint health and advises strongly to invest in a good blacksmith. Many conformational issues can be averted by having a skilled farrier right from the time they are foals. Of course, it would be remiss not to mention that prevention truly begins with nutrition. “It starts with how the broodmare is fed to prevent development of orthopaedic disease,” says Koenig. Consulting with an equine nutritionist certainly plays a role in healthy bone development and keeping horses sound.
Equine Neck CT: Advancing diagnostic precision in racehorses
Article by Rachel Tucker MRCVS
Introduction
When considering neck disorders in the racehorse, we most commonly think of severe conditions such as acute neck trauma and cervical vertebral myelopathy (Wobbler Syndrome). These represent the most severe end of the scale of orthopaedic and neurologic injury to the neck; and a diagnosis, or at least prognosis, is usually clear. However, neck conditions encompass a far wider range of clinical presentations.
Horse positioned in ct scanner
At the milder end of the scale, signs may be subtle and easily missed, whilst still being responsible for discomfort and reduced performance. The recent ability to perform a computed tomography (CT) scan of a horse’s neck represents a major advancement in our ability to diagnose neck conditions. Timely and accurate diagnosis allows efficient and targeted treatment, the ability to plan schedules and improvement in welfare through the provision of appropriate treatment and earlier return to function.
In neurologic cases, an accurate diagnosis facilitates risk management for both the horse, their handlers and riders, while improving safety for all. As conditions and injuries of the neck are being better characterised using CT, new medical and surgical treatment options are being developed, giving the potential for improved outcomes and fewer losses from the racing industry.
This article summarises how CT is being increasingly used by vets to diagnose conditions of the neck and how it is revealing previously unknown information and providing exciting new treatment opportunities.
Presentation
Conditions of the neck can cause a range of signs in the horse, which are wide-ranging in their presentation and variable in their severity. The manner in which these conditions present depends on which anatomical structures are affected. Issues affecting the bones, joints and/or soft tissues of the neck can all cause neck pain, which can manifest in a number of ways. Cases of neck pain can be severe, resulting in a horse with a rigid, fixed neck carriage, an unwillingness to walk and struggling to eat, perhaps due to a traumatic event. Neck fractures are thankfully uncommon but can be catastrophic.
More moderate signs might be displayed as a stiff neck, with reduced range of movement and resentment of ridden work. There may be pain on palpation of the neck and changes in the neck musculature. Increasingly, we are seeing horses with far more subtle signs, which are ultimately revealed to be due to neck pain and neck pathology. Typically, these horses might have an acceptable range of motion of their neck under most circumstances, but they suffer pain or restriction in certain scenarios, resulting in poor performance. This may be seen as tension through the neck, resisting rein contact, a reluctance to extend the neck over fences, or they may struggle on landing.
Riders might report a feeling of restriction or asymmetry in the mobility of the neck. In addition, these horses may be prone to forelimb tripping or show subtle forelimb lameness.
Any condition, which causes injury or disease to the spinal cord or nerves within the neck, also causes a specific range of neurologic signs. Compression of the spinal cord is most commonly caused by malformations or fractures of the cervical vertebrae, or enlargement of the adjacent articular process (facet) joints. This results in classic ‘Wobbler’ symptoms, which can range from subtle weakness and gait abnormalities, through to horses that are profoundly weak, ataxic and uncoordinated. This makes them prone to tripping, falling, or they may even become recumbent.
Peripheral nerve deficits are uncommon but become most relevant if they affect the nerves supplying the forelimbs, which can result in tripping, forelimb lameness, or local sensory deficits. This lameness might be evident only in certain circumstances, such as when ridden in a rein contact. This lameness is difficult to pinpoint as there will be no abnormality to find in the lame limb, indeed a negative response to nerve and joint blocks (diagnostic analgesia) will usually be part of the diagnostic process.
Horses can present with varying combinations and severities of neck pain, neurologic signs and peripheral nerve deficits, creating a wide range of manifestations of neck related disease.
Diagnosis
A diagnosis of neck pain is based on careful static and dynamic clinical examination and may be supported by seeing a positive response to treatment. Neurologic deficits are noted during a specific neurologic assessment, which includes a series of provocation tests such as asking a horse to walk over obstacles, back up, turn circles and walk up and down a hill. Confirming neck pathology as the cause of signs can be difficult. Until recently, radiography has been the mainstay imaging modality. Radiographs are useful for assessment of the cervical vertebrae and continue to play an important role in diagnosis; however the complex 3-dimensional shape of these bones, the large size of the neck and an inability to take orthogonal (right-angled) x-ray views means that this 2-dimensional imaging modality has significant limitations. High quality, well-positioned images are essential to maximise the diagnostic potential of radiographs.
A turning point in our diagnostic ability and understanding of neck dysfunction has been the recent adaptation of human CT scanners to allow imaging of the horse’s neck. A number of equine hospitals across the United Kingdom and Northern Europe now offer this imaging modality. We have been providing this service at Liphook Equine Hospital since 2017, with over 150 neck scans performed to date.
The CT procedure
A computed tomography (CT) scan combines a series of x-ray images taken from different angles around the area of interest to create a 3-dimensional volume of imaging data. This data is presented as a grayscale image which can be viewed in any plane and orientation. It provides excellent bone detail, and post processing techniques can provide information on soft tissue structures too. Additional techniques can be employed such as positive contrast myelography to provide greater detail about soft tissue structures. Myelography delineates the spinal cord using contrast medium injected into the subarachnoid space and is indicated in any case showing neurologic signs suggestive of spinal cord compression.
Neck CT is performed under a short general anaesthetic. Scans without myelography typically take less than 20 minutes to complete. The entire neck is imaged, from the poll to the first thoracic vertebra. The procedure is non-invasive and low risk, with anaesthetic-related complication presenting the main risk factor to the procedure. We have not encountered any significant complications in our plain CT scan caseload to date. Horses showing ataxia, weakness and incoordination (Wobbler’s), undergo CT myelography which adds around 20 minutes to the procedure. These horses are exposed to a greater level of risk due to their neurologic condition, the injection of a contrast agent and the increased chance of destabilising a more severe lesion during the procedure.
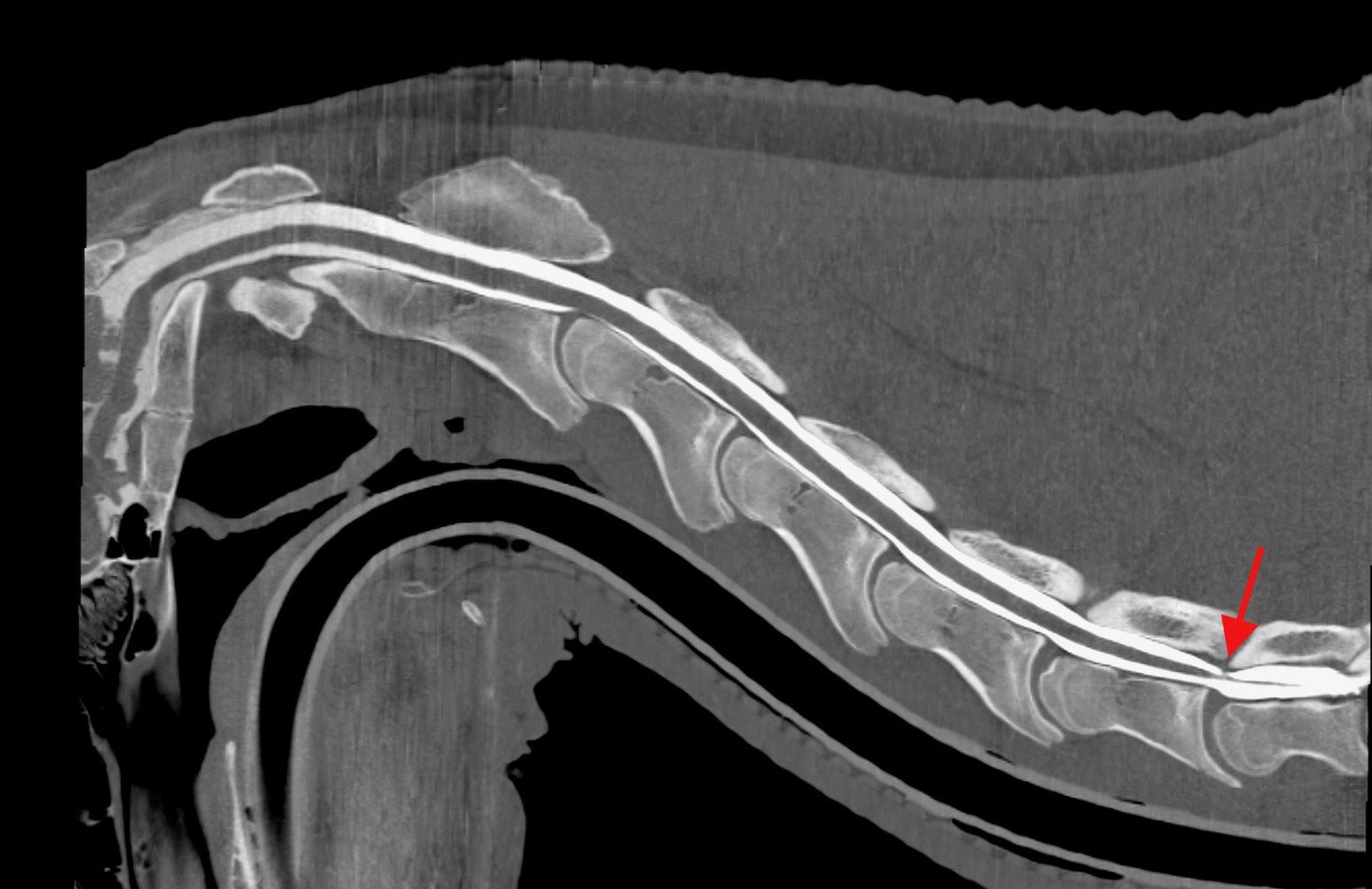
Sagittal and transverse CT myelogram images of a young racing thoroughbred showing neurologic (Wobbler) signs. shows narrowing of the spinal canal at the base of the neck (arrow)
CT is revealing more detailed information about ways that spinal cord compression can occur in Wobbler cases, about compression of spinal nerves resulting in forelimb gait deficits and precise detail about fracture configurations. It gives us detailed images of articular process joint disease, intervertebral disc disease, developmental conditions and anatomic variations. It is also revealing information about rare diseases such as vertebral abscesses or spinal neoplasia. As our caseload and confidence in the imaging modality grows, we are learning more about the value of CT in examining more subtle neck conditions. We are also bringing the benefit of a more accurate diagnosis, allowing precise targeted treatment and a better ability to provide a prognosis about outcomes—likely progression or safety factors. CT myelography allows circumferential imaging of the spinal canal and yields significantly more information than traditional x-ray myelography. As a result, we hope to enable better case selection of horses that may benefit from Wobbler surgery, with the goal of resulting in improved success rates of the surgery.
Innovations in treatment
image shows a fracture of the articular process of the 3rd cervical vertebrae in the mid neck, which was not visible on x-ray.
New treatment options are emerging as a result of our more accurate diagnoses of neck pathology. Of the first 55 horses which underwent neck CT at our hospital, we were surprised to discover that 13 (24%) had some form of osteochondral fragmentation within the articular process joints of their neck. Some of these horses were young Thoroughbreds, bred to race but showing Wobbler signs. These tended to have convincing CT evidence of type 1 CVM (Wobbler Syndrome) and osteochondrosis affecting their neck. Others had fragments which were larger and more discrete, with evidence of articular process joint enlargement/arthritis but no other bony lesions. These horses were typically older and of a range of breeds and uses.
In those horses presenting with signs of neck pain but no neurologic deficits, surgical removal of these fragments was proposed. Following further consideration and cadaver training, we have begun to offer this surgery for horses that fit the appropriate criteria and have surgically accessible fragments. We have performed arthroscopic or arthroscopic-assisted fragment removal from eight articular process joints in six horses to date. No intraoperative or postoperative complications have been encountered; and five of six horses showed complete resolution of neck pain. In the sixth horse, full recovery was not anticipated due to the presence of additional neck pathology, but partial improvement occurred for two years. Fragment removal has relieved signs of neck pain and stiffness and caused improved performance in these horses.
Two procedures that are emerging to treat spinal nerve root impingement are a targeted peripheral nerve root injection and a keyhole surgical procedure to widen the intervertebral foramen. Nerve root injection is performed in the standing sedated horse under ultrasound guidance. Surgery is performed under anaesthesia, using specialised minimally invasive equipment to widen the bony foramen using a burr. This surgery is in its infancy but offers an exciting treatment option.
Additionally, CT gives us the ability to better plan for fracture repair, undoubtedly improving our case selection for Wobbler surgery; it more accurately guides intra-articular injection of the articular process joints.
Summary
Computed tomography is transforming our ability to diagnose conditions of the horse’s neck. The procedure is low risk and now widely available in the UK and other parts of Europe. It is driving the innovation of novel treatment options with the goal of improving outcomes and reducing losses to conditions of the neck. Our CT findings are posing new questions about neck function, pain and neurologic disease and is an active area of ongoing research.
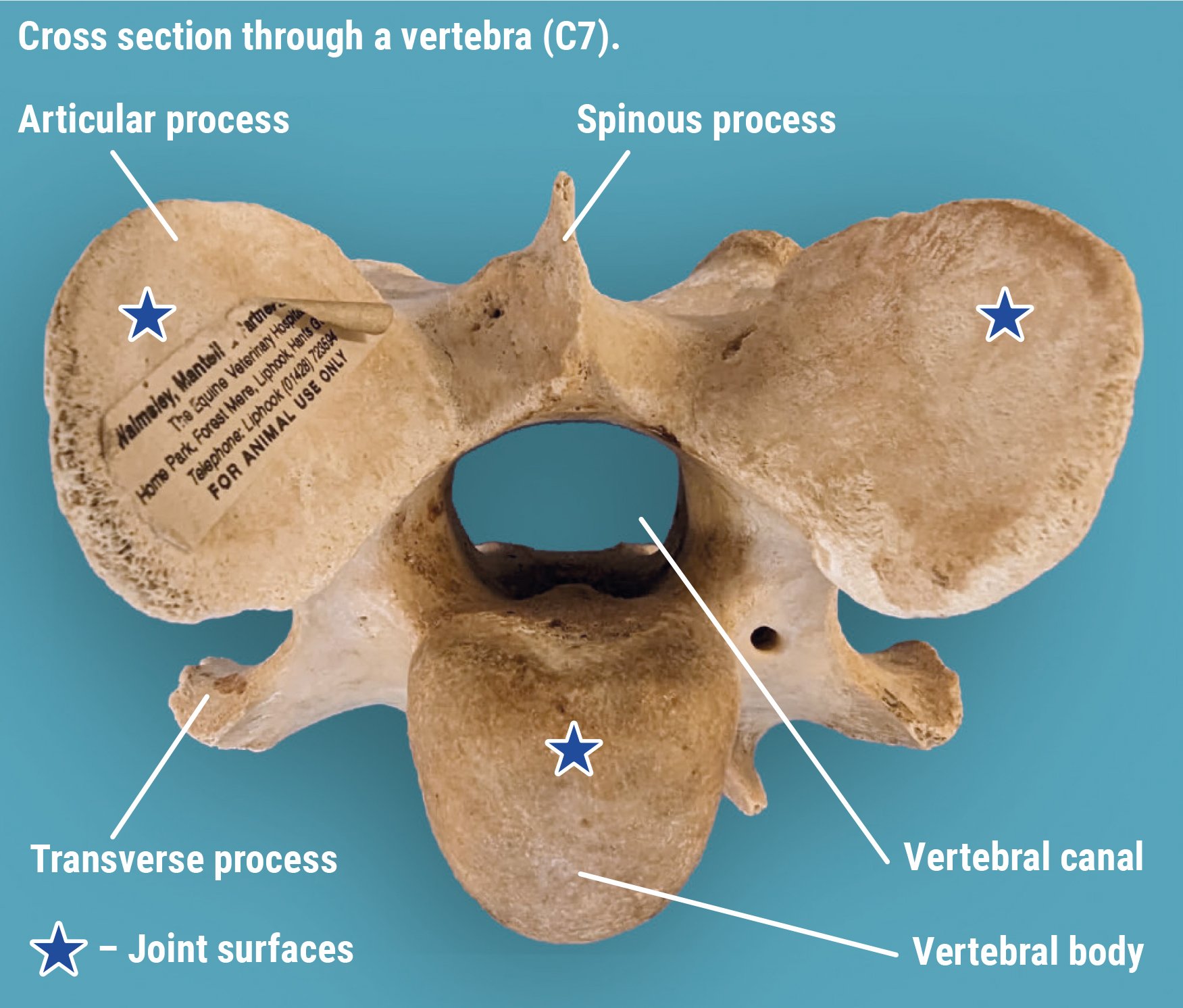
Anatomy of the cervical vertebrae
The neck vertebrae of the horse
The neck consists of seven cervical vertebrae which form a gentle S-shaped curve to link the skull at the poll to the thoracic vertebrae of the chest. Its primary functions are to protect the spinal cord, support the heavy weight of the head and to allow a large range of movement so that a horse can monitor his environment and run at speed, both being vital to this prey species.
The first (atlas) and second (axis) cervical vertebrae are highly adapted to allow head mobility. The third to sixth vertebrae are very similar in shape, whereas the seventh is shortened as it starts to show similar features to the vertebrae of the thorax. The typical cervical vertebra consists of a cylindrical column of bone (vertebral body) articulating with adjacent vertebrae via an intervertebral disc.
Running along the upper surface of this bony column is a bony canal created by the vertebral arch. This canal protects the spinal cord and associated structures that run through the centre. Above and to the side of the spinal canal sit the paired articular processes and below; and to the side sit the transverse processes. These are bony prominences to which muscles attach. The soft tissues of the neck are complex and intrinsically linked to the forelimbs and entire axial skeleton.
The articular processes also form the articular process joints (facet joints) which create an additional two joints between each vertebra. Although highly adapted, these joints are similar to others in the body consisting of cartilage-lined surfaces, a joint capsule and joint fluid. The joint surfaces are oval in shape, approximately 3-4cm in diameter and sit at an oblique angle to the neck. They provide important additional support and mobility to the neck.
References:
Schulze N., Ehrle, A., Beckmann, I and Lischer, C. (2021) Arthroscopic removal of osteochondral fragments of the cervical articular process joints in three horses. Vet Surg. ;1-9.
Swagemakers J-H, Van Daele P, Mageed M. Percutaneous full endoscopic foraminotomy for treatment of cervical spinal nerve compression in horses using a uniportal approach: Feasibility study. Equine Vet J. 2023.
Tucker R, Parker RA, Meredith LE, Hughes TK, Foote AK. Surgical removal of intra-articular loose bodies from the cervical articular process joints in 5 horses. Veterinary Surgery. 2021;1-9.
Wood AD, Sinovich M, Prutton JSW, Parker RA. Ultrasonographic guidance for perineural injections of the cervical spinal nerves in horses. Veterinary Surgery. 2021; 50:816–822.
Small wounds leading to synovial infections
Article by Peter Milner
Most experienced trainers will know from bitter experience that a seemingly tiny wound can have a big impact if a horse is unlucky enough to sustain a penetrating injury right over a critical structure like a joint capsule or tendon sheath. Collectively, joints and tendon sheaths are called synovial structures, and synovial infection is a serious, potentially career-ending and sometimes life-threatening problem.
A team of veterinary researchers from Liverpool University Veterinary School, published a study in Equine Veterinary Journal that examined factors influencing outcome and survival. This article was first published in European Trainer (issue 50 - summer 2015) but is being republished due to popular demand.
What is synovial infection?
Infection involving a synovial cavity, such as a joint or tendon sheath, is a common and potentially serious injury for the horse. The most prevalent cause is a wound, although a smaller proportion of cases result following an injection into a joint or tendon sheath, or after elective orthopaedic surgery to the area. Additionally, infection can occur via the bloodstream, particularly in foals that have not received enough colostrum. Left untreated, the horse will remain in pain, and ongoing infection and inflammation can result in permanent damage. This can ultimately result in euthanasia on welfare grounds.
What factors are important for horse survival?
When a synovial infection occurs there is a huge inflammatory response, leading to swelling and pain. The horse usually shows severe lameness but following a good clinical examination, the cause is often quickly identified. Prompt veterinary recognition of involvement of a joint or tendon sheath and aggressive treatment (involving flushing the affected synovial cavity and the correct use of systemic and local antibiotics) will often result in a good outcome for the horse. Flushing removes inflammatory debris including destructive enzymes and free radicals, and it eliminates contaminating bacteria in most cases. This is performed most effectively by arthroscopic guidance (“keyhole” surgery) under general anaesthesia. Using a “scope” to do this is considered superior to flushing through needles because arthroscopy allows the inside of the problem area to be inspected, foreign material (for example, dirt or splinters of wood) to be removed, and any concurrent damage (such as damage to the cartilage or a cut into a tendon) to be evaluated. In addition, targeted high volume lavage is best achieved via arthroscopy.
Survival following arthroscopic treatment of synovial sepsis is good – approximately 80-90% of adult horses undergoing a flush are discharged from hospital. In foals, however, the figure is much lower, at around 55%, and this likely due to complicating factors such as concurrent sepsis involving multiple organs. Our study, recently published in Equine Veterinary Journal, investigated what factors might be involved in determining survival to hospital discharge in 214 horses undergoing arthroscopic treatment for synovial sepsis. We used statistical modelling to evaluate the interactions with different factors at three key time points during the management of the condition at Liverpool Veterinary School, one of the leading UK referral veterinary hospitals. Information collected on admission to the hospital included when the horse was last seen to be normal, the cause of the infection, the degree of lameness present, and the level of white blood cells and protein in synovial fluid collected from the infected joint or tendon sheath. These lab tests are an important method which veterinarians use to determine how severe the infection is. Additional data collected included whether the surgery was performed out-of-normal working hours, if foreign material was present, the amount of inflammation present in the area, and whether any additional cartilage or tendon damage was found at surgery. Post-operative information gathered included what the levels of white blood cells and protein were in the synovial fluid after surgery and whether the horse needed further surgical treatment.
All horses in this study were greater than six months old and the majority had sustained a wound that communicated with a joint or tendon sheath. Eighty-six per cent of the 214 horses admitted to the hospital survived to hospital discharge. Of the 31 horses that did not survive, 27 were euthanised due to persistent infection or lameness.
An angry, protein-soup
A high level of protein in the synovial fluid of the affected joint or tendon sheath on admission and levels that remained high after surgery were strongly associated with a poor outcome and loss of the horse. Protein concentrations are normally fairly low in a normal joint or tendon sheath, but protein leaks into the synovial cavity from surrounding blood vessels when inflamed. Protein is also produced by cells in the synovial cavity when they are activated in response to a severe insult such as infection. Protein clots trap bacteria in the joint, making it harder to remove infection. The protein soup also includes lots of inflammatory mediators such as enzymes and signalling molecules, and these cause further inflammation, tissue damage, and sensitise pain receptors in the synovial cavity magnifying the inflammatory response and increasing the pain experienced by the horse. Unchecked, this angry, inflamed environment can result in cartilage degeneration, bone damage, and adhesion (scar) formation. This fits well with another observation from this study linking the presence of moderate or severe synovial inflammation at surgery as a negative factor for survival.
Small wounds can lead to big trouble
Interestingly, horses presenting with an obvious wound (as opposed to a small penetrating injury or no visible wound) were more likely to survive to hospital discharge. This may be due to the injury being noticed earlier and hence prompting earlier veterinary intervention. Alternatively, open wounds may allow drainage of inflammatory synovial fluid and lessen the detrimental effects of increased pressure within the joint as well as reducing ongoing exposure to inflammatory mediators. This finding highlights the fact that trainers should act promptly when faced with a wound – it is easy to underestimate just how much damage may be going on under the surface.
Horses undergoing surgical treatment of a joint or tendon sheath infection out-of-hours (for example in the middle of the night) were three times less likely to survive to hospital. Often, horses with a synovial infection arrive stressed and painful and not in an ideal state for having an anaesthetic. Early identification of an infection and appropriate management is important but stabilisation of the horse and preparation for surgery appear to outweigh any perceived benefits of undertaking immediate surgery. This is borne out by the finding that time from initial injury to treatment was not associated with outcome and is in agreement with previous findings from other researchers. It is important to reiterate that prompt recognition and treatment of a horse with an infection in a synovial cavity is essential but that surgical management within 12-24 hours of diagnosis, so that the horse is in the best condition for undergoing anaesthesia, does not affect outcome.
Do horses return to work after a synovial infection?
The big question that owners and trainers want to know is whether the horse will regain full function of the joint or tendon sheath after having an infection. Figures for return to function following surgical (arthroscopic) treatment for a synovial infection vary between 54-81%. Various factors appear to relate to outcome but when looking at a predominately thoroughbred racing population, the statistic for return to training appears to be at the higher end of this range. Factors associated with failure to return to athletic performance include the presence of thickened inflammatory tissue (known as pannus) at the time of surgery and that may relate to the development of fibrous adhesions and scar tissue within joint or tendon sheath longer-term. Some structures are particularly likely to compromise future function, and horses with an infection of the navicular bursa in the foot following a nail penetration generally do worse.
Take home message
Horses sustaining an infection to a joint or tendon sheath have a good chance of the infection clearing up and surviving the injury, with the likelihood of racing as high as around 80%. Our key message for trainers from this study is that it is essential that they recognise early when an infection involves one of these structures and have a veterinarian fully evaluate the injury. Aggressive treatment is important and involves flushing the synovial cavity using a “scope” under anaesthesia to remove as much inflammatory and infective debris as possible.